Ways To Diagnose Calcaneal Spur
Overview
Heel spurs are abnormal bony growths that develop at the back of or under the heel. Inflammation around a spur, more so than the spur itself, can cause significant pain. Fortunately, symptoms can be eased with non-surgical treatments for the vast majority of people.
Causes
Each time we take a step forward, all of our body weight first rests on the heel of one foot. As our weight moves forward, the entire foot begins to bear the body's weight, and the foot flattens and this places a great deal of pressure and strain on the plantar fascia. There is very little ?give? to the plantar fascia, so as it stretches only slightly, it pulls on its attachment to the heel. If the foot is properly aligned this pull causes no problems. However, if the foot is ?pronated?(the foot rolls outward at the ankle, causing a break down of the inner side of the shoe), the arch falls excessively, and this causes an abnormal stretching of the relatively inflexible plantar fascia, which in turn pulls abnormally hard on the heel. The same pathology occurs with ?supination? (the rolling inward of the foot, causing a break down of the outer side of the shoe). Supinated feet are relatively inflexible; usually have a high arch, and a short or tight plantar fascia. Thus as weight is transferred from the heel to the remainder of the foot, the tight plantar fascia hardly stretches at all, and pulls with great force on its attachment to the heel. In both cases, the abnormal stress placed on the attachment of the plantar fascia to the heel usually causes pain, inflammation, and possibly swelling. If this process continues, the plantar fascia partially tears away from the heel. The body will fill in this torn area with calcium; eventually it becomes bone, and a heel spur results.

Symptoms
Although it may take years to become a problem, once it appears, it may cause considerable suffering. Because of proximity to the tendons, the spur is a source of continuous painful aching. The sensation has been described as "a toothache in the foot." When you place your weight on the heel, the pain can be sufficient to immobilize you.
Diagnosis
Heel spurs and plantar fasciitis is usually diagnosed by your physiotherapist or sports doctor based on your symptoms, history and clinical examination. After confirming your heel spur or plantar fasciitis they will investigate WHY you are likely to be predisposed to heel spurs and develop a treatment plan to decrease your chance of future bouts. X-rays will show calcification or bone within the plantar fascia or at its insertion into the calcaneus. This is known as a calcaneal or heel spur. Ultrasound scans and MRI are used to identify any plantar fasciitis tears, inflammation or calcification. Pathology tests may identify spondyloarthritis, which can cause symptoms similar to plantar fasciitis.
Non Surgical Treatment
Heel spurs and plantar fascitis are usually controlled with conservative treatment. Early intervention includes stretching the calf muscles while avoiding re-injuring the plantar fascia. Decreasing or changing activities, losing excess weight, and improving the proper fitting of shoes are all important measures to decrease this common source of foot pain. Modification of footwear includes shoes with a raised heel and better arch support. Shoe orthotics recommended by a healthcare professional are often very helpful in conjunction with exercises to increase strength of the foot muscles and arch. The orthotic prevents excess pronation and lengthening of the plantar fascia and continued tearing of this structure. To aid in this reduction of inflammation, applying ice for 10-15 minutes after activities and use of anti-inflammatory medication can be helpful. Physical therapy can be beneficial with the use of heat modalities, such as ultrasound that creates a deep heat and reduces inflammation. If the pain caused by inflammation is constant, keeping the foot raised above the heart and/or compressed by wrapping with an ace bandage will help. Corticosteroid injections are also frequently used to reduce pain and inflammation. Taping can help speed the healing process by protecting the fascia from reinjury, especially during stretching and walking.
Surgical Treatment
Though conservative treatments for heel spurs work most of the time, there are some cases where we need to take your treatment to the next level. Luckily, with today?s technologies, you can still often avoid surgery. Some of the advanced technologies to treat a Heel Spur are Platelet Rich Plasma Therapy. Platelet Rich Plasma Therapy (also known as PRP) is one of several regenerative medicine techniques that University Foot and Ankle Institute has helped bring to foot and ankle care. This amazing in-office procedure allows the growth factors in the blood to be used to actually begin the healing process again long after your body has given up on healing the area. Heel Pain Shockwave Therapy. Shockwave therapy is a non-invasive procedure done in the office that allows for new blood to get to the region of fascia damage and help with healing. Results have been excellent with more than 70 percent of patients getting relief with only one treatment. Topaz for Heal Spurs and pain. Another minimally invasive technology technique is called Coblation Surgery using a Topaz probe. This minimally invasive procedure involves controlled heating of multiple tiny needles that are inserted through the skin and into the plantar fascia. This process, like PRP and Shockwave therapy, irritates the fascia enough to turn a chronic problem back into an acute problem, greatly increasing the chances of healing. Heel Spur Surgery. Endoscopic Plantar Fasciotomy is one surgical procedure that we consider to release the tight fascia. University Foot and Ankle Institute has perfected an endoscopic (camera guided) approach for fascia release to allow rapid healing and limited downtime with minimal pain.
Prevention
To prevent this condition, wearing shoes with proper arches and support is very important. Proper stretching is always a necessity, especially when there is an increase in activities or a change in running technique. It is not recommended to attempt working through the pain, as this can change a mild case of heel spurs and plantar fascitis into a long lasting and painful episode of this condition.
What Is Bursitis Of The Feet?
Retrocalcaneal bursitis is closely related to Haglund?s Deformity (or ?pump bumps?). If you have a bony enlargement on the back of the heel that rubs the Achilles tendon, it can cause the formation of a bursa (small fluid filled sack). It usually happens in athletes as shoes rub against the heel. The bursa can aggravated by the stitching of a heel counter in the shoe as well. It can make wearing shoes and exercising difficult. Another term used for this condition is ?pump bump? because it can frequently occur with wearing high heels as well. ?Retro-" means behind and ?calcaneus? means heel bone. So this is precisely where the bursitis (inflammation of the bursa) develops. Once it begins and you develop bursitis between the heel bone and the Achilles tendon, it can become even more painful. When most people first notice retrocalcaneal bursitis, it is because the skin, bursa and other soft tissues at the back of the heel gets irritated as the knot of bone rubs against the heel counter in shoes. The back of the shoes create friction and pressure that aggravate the bony enlargement and pinches the bursa while you walk.
Causes
Normally, only one bursa is in the heel, between the Achilles tendon and the heel bone (calcaneus). This bursa may become inflamed, swollen, and painful, resulting in anterior Achilles tendon bursitis. Abnormal pressure and foot dysfunction can cause a protective bursa to form between the Achilles tendon and the skin. This bursa may also become inflamed, swollen, and painful, resulting in posterior Achilles tendon bursitis.
Symptoms
Pain or tenderness at the back of the heel around the Achilles region. Increased pain during activities with strong, repetitive calf contractions, walking (uphill), stair climbing, running, jumping. Pain may be worse with rest after activity (that night or the next morning) or at the beginning of the excercise. Pain when wearing shoes and the heel is getting rubbed. Bump forming on the back of the heel. Limping. Stiffness. Decreased range of motion. Redness and warmth (if the bursa gets infected).
Diagnosis
The doctor will discuss your symptoms and visually assess the bones and soft tissue in your foot. If a soft tissue injury is suspected, an MRI will likely be done to view where and how much the damage is in your ankle. An x-ray may be recommended to rule out a bone spur or other foreign body as the cause of your ankle pain. As the subcutaneous bursa is close to the surface of the skin, it is more susceptible to septic, or infectious, bursitis caused by a cut or scrape at the back of the heel. Septic bursitis required antibiotics to get rid of the infection. Your doctor will be able to determine whether there is an infection or not by drawing a small sample of the bursa fluid with a needle.
Non Surgical Treatment
The patient with retrocalcaneal bursitis should be instructed to apply ice to the posterior heel and ankle in the acute period of the bursitis. Icing can be performed several times a day, for 15-20 minutes each. Some clinicians also advocate the use of contrast baths. Gradual progressive stretching of the Achilles tendon may help relieve impingement on the subtendinous bursa and can be performed in the following manner. Stand in front of a wall, with the affected foot flat on the floor. Lean forward toward the wall until a gentle stretching is felt within the ipsilateral Achilles tendon. Maintain the stretch for 20-60 seconds and then relax. Perform the stretches with the knee extended and then again with the knee flexed. To maximize the benefit of the stretching program, repeat the above steps for several stretches per set, several times daily. Avoid ballistic (ie, abrupt, jerking) stretches. Other treatment options are microcurrent therapy and corticosteriod injection into the retrocalcaneal bursa. If conservation treatment fails then surgery is indicated.
Surgical Treatment
Bursectomy is a surgical procedure used to remove an inflamed or infected bursa, which is a fluid-filled sac that reduces friction between tissues of the body. Because retrocalcaneal bursitis can cause chronic inflammation, pain and discomfort, bursectomy may be used as a treatment for the condition when it is persistent and cannot be relived with other treatments. During this procedure, a surgeon makes small incisions so that a camera may be inserted into the joint. This camera is called an arthroscope. Another small incision is made so that surgical instruments can be inserted to remove the inflamed bursa.
Could Neuropathy Cause Hammertoes
Many disorders can affect the joints in the toes, causing pain and preventing the foot from functioning as it should. A hammertoe occurs when the joint at the end of the toe cannot straighten. Excessive rubbing of the hammer toe against the top of the shoe can lead to pain and the development Hammer toes of a corn. The tip of the toe is often turned down against the shoe causing pressure and discomfort.
Causes
Hammer toes are most frequently caused by a muscle - tendon imbalance in the foot, and are seen both in adults and children. Foot muscles work in pairs to straighten and bend the toes. If your foot has a biomechanical defect, the muscles tighten and the tendons shorten. Eventually, the toe muscles can?t straighten the toe, even when barefoot. Contributing factors are poor choices in footwear, arthritis, or trauma.
 Symptoms
Symptoms
Hammertoe and mallet toe feature an abnormal bend in the joints of one or more of your toes. Moving the affected toe may be difficult or painful. Corns and calluses can result from the toe rubbing against the inside of your shoes. See your doctor if you have persistent foot pain that affects your ability to walk properly.
Diagnosis
A hammertoe is usually diagnosed with a physical inspection of your toe. Imaging tests, such as X-rays, may be ordered if you have had a bone, muscle, or ligament injury in your toe.
Non Surgical Treatment
Conservative treatment is the first choice, often starting with a change of shoes to ones that have soft, larger toe spaces. Toe exercises may be prescribed to stretch and strengthen the toe muscles. Over-the-counter straps, cushions or non-medicated corn pads may be recommended to help relieve your symptoms.
Surgical Treatment
There are generally two methods surgeons use to correct hammer toes, they are joint resection (arthroplasty) or bone mending (fusion), and the location where this is performed on the toe depends on where the toe is buckled. Its important to recognize that most of the surgical work involved the joints of the toe, not the joint of the ball of the foot. Sometimes a toe relocation procedure is needed when the joint of the ball of the foot is malaligned (subluxed or dislocated).
 Prevention
Prevention
The best treatment is good prevention! Hammertoe can be prevented by wearing shoes with ample toe room, avoiding high heels, and wearing adjustable shoes to assure a looser fit. When buying shoes, shop at the end of the day when your feet are swollen from daily activity, try both shoes on to confirm they fit properly, and if necessary, visit a shoe repair store to see if they can stretch your shoes for a better fit.
How To Treat Hammer Toes Without Surgery
 Overview
Overview
The smallest four toes of each foot have three bony segments connected by two joints, just as the fingers do. Hammer toes is a deformity in which one or more of the small toes develops a bend at the joint between the first and second segments so that the tip of the toe turns downward, making it looks like a hammer or claw. The second toe is affected most often.
Causes
Certain risk factors increase your likelihood of developing a hammertoe. These include a family history of hammertoes, wearing tight or pointy-toed shoes, wearing shoes that are too small, having calluses, bunions, or corns (thickened layers of skin caused by prolonged/repeated friction) Wearing shoes that are too small can force the joint of your toes into a dislocated position. This makes it impossible for your muscles to stretch out. Over time, the practice of wearing improperly fitting shoes increases your risk of developing hammertoes, blisters, bunions, and corns.
 Symptoms
Symptoms
Here is a look at some of the symptoms hammertoe can cause. They include hammer-like or claw-like appearance of the toe. Pain when walking or moving the foot. Difficulty moving the toe. Corns may form on top of the toe. Callus may form on the sole of the foot. During the initial stages, you may hammertoe be able to manually straighten your toe. This is called a flexible hammertoe. But as time passes, the toe will not move as easily and will continue to look like a hammer. Pressure and irritation over the joint can cause a blister to develop and become a corn over time. These corns have the potential to become infected and cause additional symptoms such as redness, bleeding, and difficulty wearing shoes and socks. Corns are the main cause of pain when hammertoes are developing.
Diagnosis
A hammertoe is usually diagnosed with a physical inspection of your toe. Imaging tests, such as X-rays, may be ordered if you have had a bone, muscle, or ligament injury in your toe.
Non Surgical Treatment
Your podiatrist may recommend one or more of these treatments to manage your hammer toes. Wear shoes with roomy toe boxes which don?t force your toes together. Exercises to stretch and strengthen muscles in the toes. Over the counter toe straps, cushions, and corn pads. Custom orthotic inserts. Toe caps or toe slings. In severe cases, surgery to release the muscles in the affected toes.
Surgical Treatment
Surgery may not help how your foot looks. And your toe problems may also come back after surgery. This is more likely if you keep wearing the kinds of shoes that cause toe problems. Your expectations will play a large role in how you feel about the results of surgery. If you are only having surgery to improve the way your foot looks, you may not be happy with how it turns out.
 Prevention
Prevention
Be good to your feet, because they carry you. They are designed to last a lifetime, but that doesn?t mean they don?t need some love and care as well as some basic maintenance. Check your feet regularly for problems. This is especially true if you have diabetes or any other medical condition that causes poor circulation or numbness in your toes. If you do, check your feet every day so problems can be caught early on. Good circulation is essential. When you're sitting down, put your feet up. If you've been sitting for a while, stretch your legs and feet. Give yourself a foot massage, or ask someone you love for a foot massage. A warm foot bath is also a good idea.
Bunions Cause And Effect
Overview
 A bunion is generally considered as an enlargement of the joint (a lump of bone) at the base and side of the big toe (specifically, the first metatarsophalangeal joint). Bunions form when the toe moves out of place. As the big toe bends towards the others this lump becomes larger and the bunion can become painful, arthritis and stiffness can eventually develop. Hallux valgus or hallux abducto valgus (HAV) is the name used for the deviated position of the big toe and a bunion refers to the enlargement of the joint, most of the time the two go together and can just be referred to as 'bunions'. The word bunion is from the Latin "bunion," meaning enlargement.
A bunion is generally considered as an enlargement of the joint (a lump of bone) at the base and side of the big toe (specifically, the first metatarsophalangeal joint). Bunions form when the toe moves out of place. As the big toe bends towards the others this lump becomes larger and the bunion can become painful, arthritis and stiffness can eventually develop. Hallux valgus or hallux abducto valgus (HAV) is the name used for the deviated position of the big toe and a bunion refers to the enlargement of the joint, most of the time the two go together and can just be referred to as 'bunions'. The word bunion is from the Latin "bunion," meaning enlargement.
Causes
Bunions are sometimes genetic and consist of certain tendons, ligaments, and supportive structures of the first metatarsal that are positioned differently. This bio-mechanical anomaly may be caused by a variety of conditions intrinsic to the structure of the foot, such as flat feet, excessive flexibility of ligaments, abnormal bone structure, and certain neurological conditions. These factors are often considered genetic. Although some experts are convinced that poor-fitting footwear is the main cause of bunion formation, other sources concede that footwear only exacerbates the problem caused by the original genetic structure. Bunions are commonly associated with a deviated position of the big toe toward the second toe, and the deviation in the angle between the first and second metatarsal bones of the foot. The small sesamoid bones found beneath the first metatarsal (which help the flexor tendon bend the big toe downwards) may also become deviated over time as the first metatarsal bone drifts away from its normal position. Arthritis of the big toe joint, diminished and/or altered range of motion, and discomfort with pressure applied to the bump or with motion of the joint, may all accompany bunion development. Atop of the first metatarsal head either medially or dorso-medially, there can also arise a bursa that when inflamed (bursitis), can be the most painful aspect of the process.
Symptoms
The most common symptoms associated with this condition are pain on the side of the foot just behind the great toe. A red painful bump is usually present. Pain is usually brought on with walking or sports. Shoes don't cause bunions but will typically aggravate them. Stiff leather shoes or shoes with a tapered toe box are the prime offenders. This is why bunion pain is most common in women whose shoes have a pointed toe box. The bunion site will often be slightly swollen and red from the constant rubbing and irritation of a shoe. Occasionally, corns can develop between the 1st and 2nd toe from the pressure the toes rubbing against each other.
Diagnosis
Most patients are diagnosed to have bunions from clinical history and examination. However, in some cases, X-rays will be performed to determine the extent of damage to the joint. Furthermore, it will enable the treating doctor to decide on the best course of management of the patient.
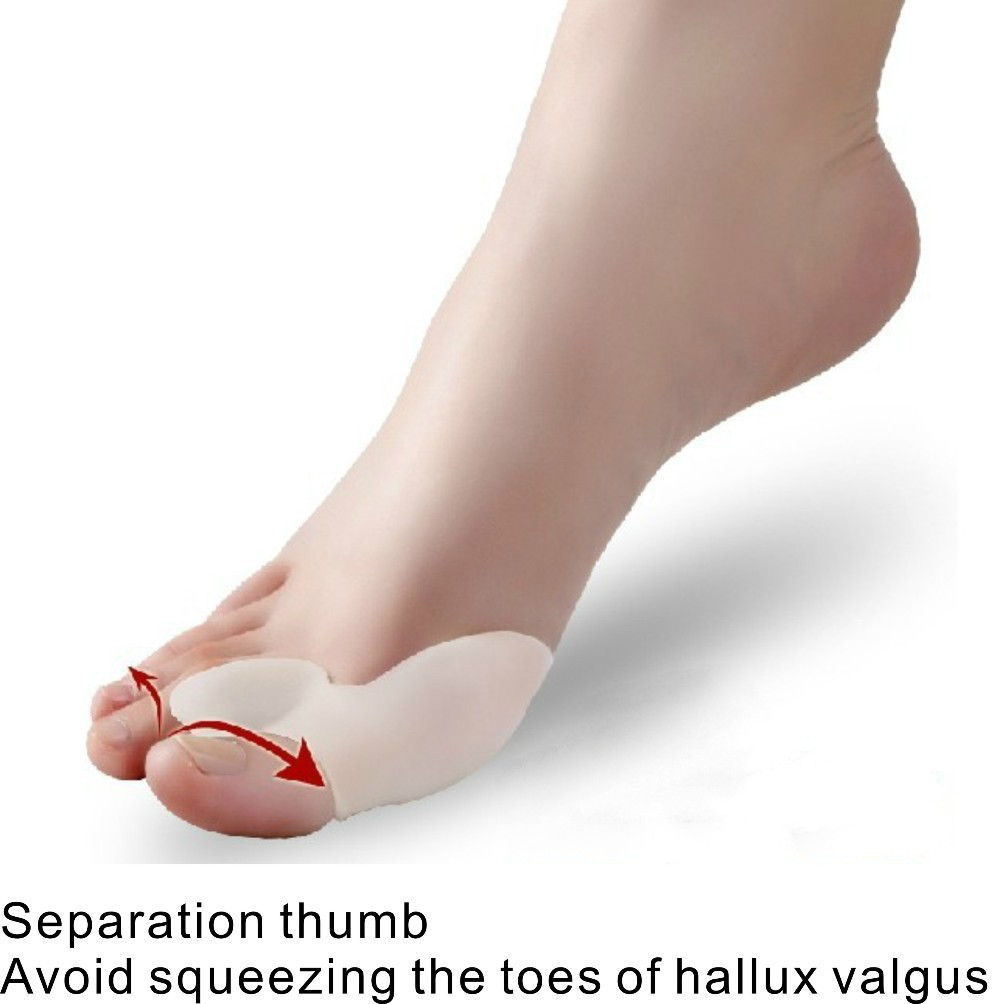
Non Surgical Treatment
Sometimes observation of the bunion is all that?s needed. To reduce the chance of damage to the joint, periodic evaluation and x-rays by your surgeon are advised. In many other cases, however, some type of treatment is needed. Early treatments are aimed at easing the pain of bunions, but they won?t reverse the deformity itself. These include changes in shoewear. Wearing the right kind of shoes is very important. Choose shoes that have a wide toe box and forgo those with pointed toes or high heels which may aggravate the condition. Padding. Pads placed over the area of the bunion can help minimize pain. These can be obtained from your surgeon or purchased at a drug store. Activity modifications. Avoid activity that causes bunion pain, including standing for long periods of time. Medications. Oral nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, may be recommended to reduce pain and inflammation. Icing. Applying an ice pack several times a day helps reduce inflammation and pain. Injection therapy. Although rarely used in bunion treatment, injections of corticosteroids may be useful in treating the inflamed bursa (fluid-filled sac located around a joint) sometimes seen with bunions. Orthotic devices. In some cases, custom orthotic devices may be provided by the foot and ankle surgeon. 
Surgical Treatment
When the pain of a bunion interferes with daily activities, and conservative treatment has been completed it's time to discuss surgical options. Foot Mechanics has excellent relationships with many Orthopaedic Surgeons, who are the specialists who perform bunion surgery. Because bunions are caused by faulty foot mechanics surgery can improve the look of your feet by removing the ?bump? but if the underlying mechanics are not addressed then the bunion is likely to return. For this reason orthotics are used post-surgery to prevent the return of bunions.
The Truth Regarding Over-Pronation
One of the most common causes of foot and leg discomfort is a condition known as overpronation. Normal pronation, or "turning inward" of the foot is necessary as the foot adapts to the ground. With over pronation, the arch flattens, collapses, and soft tissues stretch. This causes the joint surfaces to function at unnatural angles to each other. When this happens, joints that should be stable now become very loose and flexible. At first, over pronation may cause fatigue. As the problem gets worse, strain on the muscles, tendons, and ligaments of the foot and lower leg can cause permanent problems and deformities.
Causes
Over-pronation is very prominent in people who have flexible, flat feet. The framework of the foot begins to collapse, causing the foot to flatten and adding stress to other parts of the foot. As a result, over-pronation, often leads to Plantar Fasciitis, Heel Spurs, Metatarsalgia, Post-tib Tendonitis and/or Bunions. There are many causes of flat feet. Obesity, pregnancy or repetitive pounding on a hard surface can weaken the arch leading to over-pronation. Often people with flat feet do not experience discomfort immediately, and some never suffer from any discomfort at all. However, when symptoms develop and become painful, walking becomes awkward and causes increased strain on the feet and calves.
Symptoms
Common conditions that develop with prolonged overpronation typically include plantar fasciitis, achilles tendonitis, shin splints, posterior tibial stress syndrome and even IT band syndrome. With long term neglect you may see the development of bunyons, foot deformities and early onset of hip and knee arthritis.
Diagnosis
The best way to discover whether you have a normal gait, or if you overpronate, is to visit a specialty run shop, an exercise physiologist, a podiatrist or a physical therapist who specializes in working with athletes. A professional can analyze your gait, by watching you either walk or run, preferably on a treadmill. Some facilities can videotape your gait, then analyze the movement of your feet in slow-motion. Another (and less costly) way is to look at the bottom of an older pair of run shoes. Check the wear pattern. A person with a normal gait will generally see wear evenly across the heel and front of the shoe. A person who overpronates will likely see more wear on the OUTside of the heel and more wear on the INside of the forefoot (at the ball). A person who supinates will see wear all along the outer edges of the shoe. You can also learn about your gait by looking at your arches. Look at the shape your wet feet leave on a piece of paper or a flat walking surface.

Non Surgical Treatment
The way a foot orthotic works is by altering the weight-bearing surface of the foot. The simulated foot improvement is only possible when standing still with full weight applied. Orthotics are of little help through most of the actual walking cycle. observationPatients may experience some symptom relief, but the orthotic cannot correct the internal osseous misalignment. Over-the-counter foot orthotics are usually of little help and wear out quickly. Custom-made foot orthotics, obtained through your doctor's office, are generally expensive. Though they last longer and have less chance of ill-effects than OTC brands, they still need to be replaced often. Over a lifetime, an individual can spend several thousands of dollars in total costs associated with orthotics and see little or no results. This is because orthotics only work when you are wearing them and do not treat the cause of the problem. In many cases, the external pressure points created by orthotics can cause more problems than solutions. Blisters, sore feet, sore joints and many other long-term complications can arise as a consequence of wearing orthotics.
Prevention
Duck stance: Stand with your heels together and feet turned out. Tighten the buttock muscles, slightly tilt your pelvis forwards and try to rotate your legs outwards. You should feel your arches rising while you do this exercise.
Calf stretch:Stand facing a wall and place hands on it for support. Lean forwards until stretch is felt in the calves. Hold for 30 seconds. Bend at knees and hold for a further 30 seconds. Repeat 5 times.
Golf ball:While drawing your toes upwards towards your shins, roll a golf ball under the foot between 30 and 60 seconds. If you find a painful point, keep rolling the ball on that spot for 10 seconds.
Big toe push: Stand with your ankles in a neutral position (without rolling the foot inwards). Push down with your big toe but do not let the ankle roll inwards or the arch collapse. Hold for 5 seconds. Repeat 10 times. Build up to longer times and fewer repetitions.
Ankle strengthener: Place a ball between your foot and a wall. Sitting down and keeping your toes pointed upwards, press the outside of the foot against the ball, as though pushing it into the wall. Hold for 5 seconds and repeat 10 times.
Arch strengthener: Stand on one foot on the floor. The movements needed to remain balanced will strengthen the arch. When you are able to balance for 30 seconds, start doing this exercise using a wobble board.
What Exactly Is Severs Disease?
Severs? disease usually presents with pain in either one or both of a sufferer?s heels. The area can be sore or tender, particularly first thing in the morning or after squeezing. Because the pain is focussed on the heel, an important part of the foot that makes contact with the ground through virtually all movement, sufferers often have to limp to alleviate their discomfort. The pain of Severs? disease is at its worst after any exertion that involves contact between a heel and the ground, particularly strenuous exercise like running or sport. The condition is caused by the wear and tear of structures in the heel, most significantly the heel bone and any attached tendons. Severs? disease is prevalent in young children who are extremely active, particularly as the heel and its attached tendons are still growing in the age group the condition most commonly affects (7-14).
Causes
At birth, most of our foot bones are still made of cartilage, which ossifies (becomes bony) over the first few years of life. At the back of the heel, there is a growth plate that is attached to the main body of the heel bone by a cartilaginous join. At about the age of 14-15 years, this area of cartilage between the growth plate and the heel bone ossifies, fusing the area to the heel. Sever?s disease occurs when there is too much motion or strain across the growth plate, resulting in this area becoming inflamed and painful.
Symptoms
The patient complains of activity related pain that usually settles with rest. On Examination the heel bone - or calcaneum - is tender on one or both sides. The gastrocnemius and soleus muscles (calf muscles) may be tight and bending of the ankle might be limited because of that. Foot pronation (rolling in) often exacerbates the problem. There is rarely anything to see and with no redness or swelling and a pain that comes and goes mum and dad often wait before seeking advice on this condition. The pain may come on partway through a game and get worse or come at the end of the game. Initially pain will be related only to activity but as it gets worse the soreness will still be there the next morning and the child might limp on first getting up.
Diagnosis
A doctor or other health professional such as a physiotherapist can diagnose Sever?s disease by asking the young person to describe their symptoms and by conducting a physical examination. In some instances, an x-ray may be necessary to rule out other causes of heel pain, such as heel fractures. Sever?s disease does not show on an x-ray because the damage is in the cartilage.
Non Surgical Treatment
Cold packs: Apply ice or cold packs to the back of the heels for around 15 minutes after any physical activity, including walking.
Shoe inserts: Small heel inserts worn inside the shoes can take some of the traction pressure off the Achilles tendons. This will only be required in the short term.
Medication: Pain-relieving medication may help in extreme cases, but should always be combined with other treatment and following consultation with your doctor).
Anti-inflammatory creams: Also an effective management tool.
Splinting or casting: In severe cases, it may be necessary to immobilise the lower leg using a splint or cast, but this is rare.
Time: Generally the pain will ease in one to two weeks, although there may be flare-ups from time to time.
Correction of any biomechanical issues: A physiotherapist can identify and discuss any biomechanical issues that may cause or worsen the condition.
Education: Education on how to self-manage the symptoms and flare-ups of Sever?s disease is an essential part of the treatment.
Surgical Treatment
The surgeon may select one or more of the following options to treat calcaneal apophysitis. Reduce activity. The child needs to reduce or stop any activity that causes pain. Support the heel. Temporary shoe inserts or custom orthotic devices may provide support for the heel. Medications. Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, help reduce the pain and inflammation. Physical therapy. Stretching or physical therapy modalities are sometimes used to promote healing of the inflamed issue. Immobilization. In some severe cases of pediatric heel pain, a cast may be used to promote healing while keeping the foot and ankle totally immobile. Often heel pain in children returns after it has been treated because the heel bone is still growing. Recurrence of heel pain may be a sign of calcaneal apophysitis, or it may indicate a different problem. If your child has a repeat bout of heel pain, be sure to make an appointment with your foot and ankle surgeon.